In this inaugural edition of our newsletter, we are looking at what has been accomplished thus far in creating a medical campus in Cape Breton. The progress has been significant, and while there is a great deal of work ahead, we are building on a strong foundation, and an even stronger partnership.
A Memorandum of Understanding (MOU) has been signed between Cape Breton University and Dalhousie Medical School. It outlines the framework under which we will operate and establishes the Cape Breton Medical Campus Steering Committee, which is tasked with addressing the operational matters related to the campus. We believe this partnership has great potential to provide excellent medical education that will benefit Cape Breton and all of Nova Scotia for years to come.
The Province of Nova Scotia has also proven to be an important partner in the undertaking. On January 27, 2023, Premier Tim Houston announced the medical campus would become a reality.
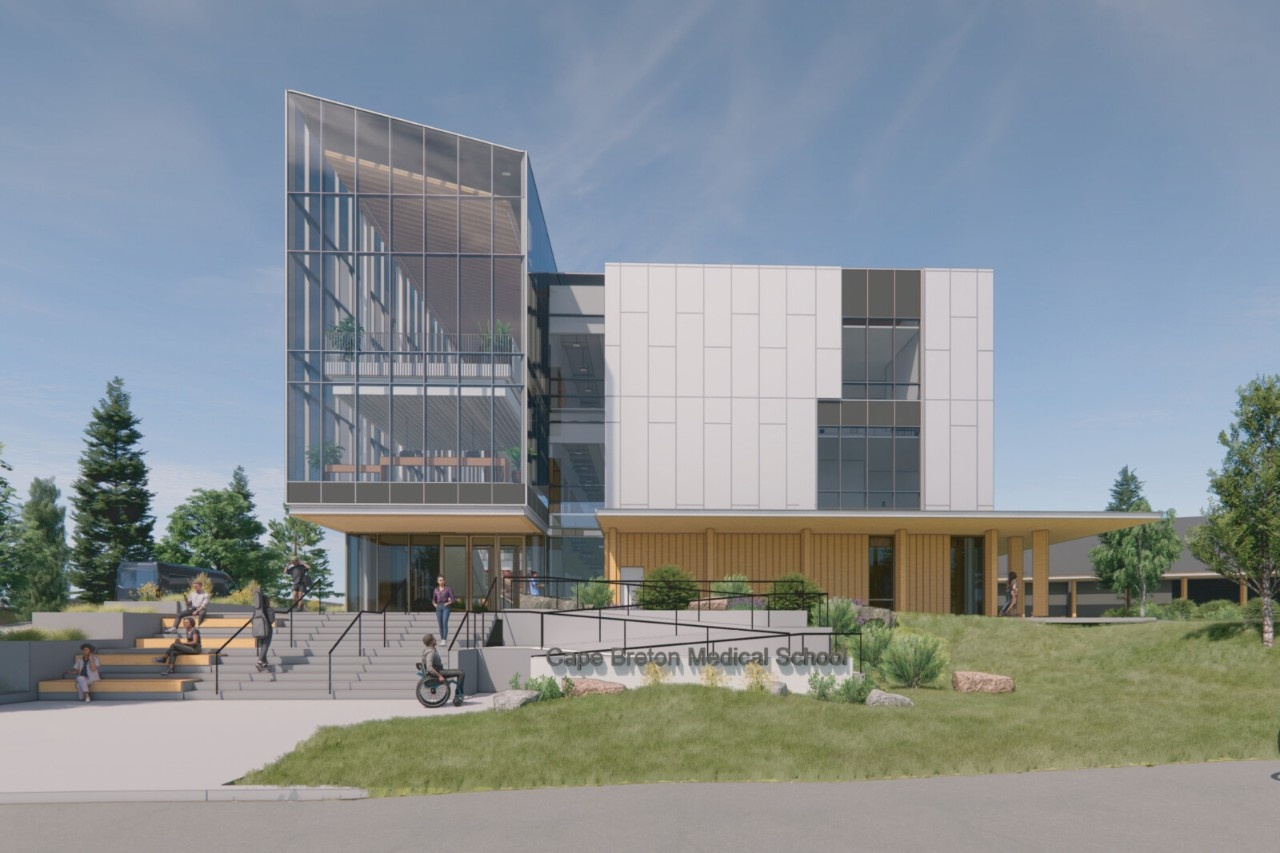
Premier Houston travelled to Cape Breton again on March 7, 2023 to announce a $58.9 million investment in the medical campus, including a $49 million investment for the creation of a medical sciences centre, $6.2 million for the creation of a 10,000-patient collaborative clinic, and $3.7 million for the expansion of the health and counselling centre at CBU.
We very much understand there is a great deal of work ongoing within several health facilities here in Cape Breton. That is why our steering committee is committed to working with the Health Redevelopment Team to ensure our mutual needs are aligned and complementary.
Transparency as we continue to progress is important. To that end, we intend to keep our stakeholders, partners, and the community informed through regular updates.
Key Appointments Named for CBMC
Three well-known health professionals will take on leadership roles at the Cape Breton Medical Campus.
 Dr. Kevin Orrell has been appointed Interim Associate Dean, while Dr. Susan MacLeod and Dr. Jim MacKillop will become Family Medicine Special Advisors. The appointments were announced by David C. Dingwall, President and Vice-Chancellor of Cape Breton University and Dr. David Anderson, Dean of the Faculty of Medicine at Dalhousie.
Dr. Kevin Orrell has been appointed Interim Associate Dean, while Dr. Susan MacLeod and Dr. Jim MacKillop will become Family Medicine Special Advisors. The appointments were announced by David C. Dingwall, President and Vice-Chancellor of Cape Breton University and Dr. David Anderson, Dean of the Faculty of Medicine at Dalhousie.
Working with the Interim Associate Dean, the Family Medicine Advisors will engage and liaise with family doctors, other physicians, and health professionals regarding the Cape Breton Medical Campus. They will also advise on family medicine and rural and remote health strategy for the new campus, and will engage with stakeholders and partners on its family medicine focus.
Dr. Orrell has been serving as the Special Advisor to the president of Cape Breton University on strategic health initiatives, including the Cape Breton Medical Campus, and is a skilled physician and orthopedic surgeon. He is the former Deputy Minister of the Provincial Department of Health and Wellness where he was instrumental in overseeing the provincial response to Covid-19.
Dr. Susan MacLeod is a graduate of Memorial University (MUN) and has been practicing family medicine for 21 years. She continues to welcome students as an assistant professor with Dalhousie University.
Dr. Jim MacKillop graduated from Dalhousie University in 1981 and began practicing family medicine in Sydney in 1984. He was the inaugural site lead for Dalhousie's Cape Breton Family Medicine Residency Program from its beginning in 1997 until 2014, and continues as an assistant professor at Dalhousie University. Dr. MacKillop currently practices family medicine at the Sydney Primary Care Medical Clinic Collaborative.
Engaging Physicians
In early June, leaders of the Faculty of Medicine at Dalhousie University and Cape Breton University held three sessions with physicians in Cape Breton to discuss the new medical campus. Information sessions were held in Sydney, Cheticamp and Inverness and included a presentation by Dr. David Anderson, Dean of the Faculty of Medicine and Dr. Kevin Orrell, Associate Dean of the Cape Breton Medical Campus.
Participants learned about the program, the curriculum and how to get involved with the new campus, and additional sessions will be planned for the future as work on the medical campus continues.
Watch the presentation
Pilot Program Extended
After the success of the first medical education pilot initiative, another five seats will be offered for 2023. The Medical Education Pilot Initiative was initiated by Cape Breton and Dalhousie Universities to test whether Nova Scotians would respond to a different approach to medical school admissions. That approach includes geographic and program of focus criteria, along with a return of service provision.
The program began in September 2022, and saw CBU sponsor five seats at Dalhousie’s Faculty of Medicine MD Program for qualified rural Nova Scotian applicants including Cape Breton, Mi’kmaq, and other Indigenous and African Nova Scotian individuals.
CBU and the Government of Nova Scotia, with partners at Dalhousie, are working together to find innovative and creative ways to increase access to family doctors in rural Nova Scotia, including creating a medical campus in Cape Breton. The five successful students have committed to a return of service criteria with a focus on family medicine and working in rural Nova Scotia for five years after completing their degree. Students will graduate with a Doctor of Medicine from Dalhousie University, and efforts have been made to create more capacity for residencies in rural Nova Scotia.
Cape Breton University will collaborate with Dalhousie University to choose students from the Dalhousie Medical School wait list for the 2023-24 academic year to fill the seats.

In Pursuit of Childhood Dreams: Meet Abe Chidac
Childhood dreams may not always come true, but when they do, they mean something extra special. Abe Chidiac is one of the lucky ones who is making his childhood dream come true as he studies Medicine at Dalhousie University.
Abe is one of five students selected for Cape Breton University and Dalhousie University’s Medical Education Pilot Initiative aimed at innovative and creative solutions to alleviate physician shortages in rural Nova Scotia.
Growing up in Shelburne, a rural town on the southern shore of Nova Scotia, Abe was able to experience firsthand how a lack of healthcare and education impacts communities in Canada. Abe’s parents immigrated to Canada from Lebanon, giving Abe the chance to experience the healthcare landscape in Lebanon during trips to visit family. Both of these experiences motivated him to pursue a career in the medical field with the goal of helping people at their most vulnerable.
After working as a recreational therapist, and volunteering at the IWK, being accepted into the Medical Education Pilot Initiative was an exciting step for Abe. “It took me months to fathom that I had actually been accepted into the program,” he says. “I am very grateful for the opportunity to pursue my dreams.”
Before enrolling in the medical program, Abe graduated in 2021 with a Bachelor of Science with honours in Medical Sciences from Dalhousie University. His honours thesis focused on self-help internet-delivered cognitive behavioural therapy (CBTi) for insomnia. Throughout high school and university, Abe also volunteered and worked diligently to help communities in need. He travelled to places like Nicaragua and Ecuador where he helped to build schools, allowing him to gain further insight on the importance of healthcare education. He says he is grateful for every life experience that led him to the path of becoming an MD.
Thinking of his own experience growing up in rural Nova Scotia, Abe explains that at times, people would have to travel over two hours to get the healthcare they need. “There are so many people in our town without a family doctor, which is a gateway to a solid healthcare system,” explains Abe. “Improving access to healthcare in a province like Nova Scotia, which has many rural communities, is of utmost importance. It is unjust that those living further away from a city are struggling to get the care they need.”
Abe says the MD program has already equipped him with countless skills he will utilize throughout his career as a doctor. “The opportunity to connect with physicians has provided me with important knowledge, in particular, the Skilled Clinician course,” he shares. “This course has shown me how to interact with patients, perform physical exams and the integration of important factors such as socioeconomic status in medical history to ensure the best care for everyone.”
Throughout Abe’s journey, his family has served as a major support system. “Watching their reactions when I was accepted into medical school felt surreal, as they had experienced every emotion I did while going through the application cycle,” says Abe. “I would not be here without all of their support.”
Abe considers himself very fortunate to be able to pursue his lifelong goals of becoming a doctor and helping the most vulnerable. Learn more about the Cape Breton University and Dalhousie University’s Medical Education Pilot Initiative.