Meet researcher, Dr. Gabriela Ilie

An Associate Professor in the Department of Community Health & Epidemiology, jointly appointed in the Department of Urology, with cross-appointments in Radiation Oncology and Psychology & Neuroscience, Dr. Gabriela Ilie is a nationally and internationally recognized leader in cancer survivorship, digital health innovation, and patient empowerment. She holds the Soillse Endowed Scientist position in Cancer Quality of Life Research and serves as Director of the Soillse Research Lab for Cancer Survivorship & Patient Empowerment, an initiative made possible through the vision and generosity of Frank and Debbi Sobey. Her work tackles a longstanding gap in oncology: ensuring that supportive care is comprehensive, accessible, and focused on the whole person from diagnosis through long‑term survivorship. Through home‑based, digital empowerment programs, PC‑PEP, CancerPEP, PictouPEP, and the forthcoming BreastCancerPEP Phase III randomized controlled trial—she helps patients rebuild physical, emotional, and relational well‑being with daily, structured guidance delivered via short videos, meditations, strength training, sleep strategies, and communication tools.
Grounded in health equity, these programs prioritize Indigenous, Black, LGBTQ+, rural, and underserved communities. Each year, her lab partners with more than 50 Canadian organizations and over 10 international collaborators including groups like Movember, the Walnut Foundation, Prostate Cancer Foundation BC, Nova Scotia Health’s Brotherhood and Sisterhood networks, Congress of Aboriginal People and collaborators in Europe, Africa, Australia, and New Zealand, ensuring that survivorship support reaches populations historically overlooked in cancer care.
Dr. Ilie’s approach combines scientific rigor with human connection. She views healing as relational and rooted in meaning, joy, and community. Her work is redefining survivorship as an essential component of cancer care, influencing policy and practice through national trials, global partnerships, and innovative digital tools.
The impact of this work has been recognized with the 2024 Public Impact Award from Research Nova Scotia and the 2025 Canadian Association for Psychosocial Oncology Innovation Award, honoring scalable, evidence‑based programs that measurably improve quality of life and mental health outcomes for cancer survivors.
Dr. Ilie’s philosophy is deeply human: “We are here to add life to living, not just years to life.”
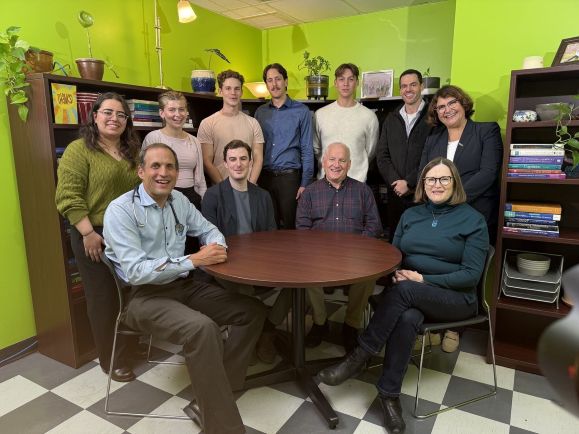
In practice, that means integrating mindfulness and gratitude practices, relational exercises, sleep hygiene, and purpose‑building into daily routines—anchoring clinical excellence in joy, play, meaning, and connection. Alongside a vibrant mentoring portfolio that spans MSc and PhD trainees, medical residents, postdoctoral fellows, and undergraduate learners, Dr. Gabriela Ilie also advances public education through community sessions, patient podcasts, annual newsletters, and the documentary Empower, with resources available at pcpep.org.
Q: What does “cancer survivorship” mean to you—and why does it matter?
For me, survivorship begins the day a person is diagnosed and continues throughout their life. It isn’t limited to physical recovery; it encompasses emotional well‑being, psychological resilience, sleep, sexuality, identity, relationships, and the social realities that accompany cancer. Modern oncology has extended survival, but quality of life often lags behind. Too many people feel anxious, overwhelmed, or unsure how to rebuild. My work is about ensuring that individuals don’t simply survive—they have the knowledge, confidence, and community to live well, regain control, and rediscover joy.
Q: How do your empowerment programs help people feel in control—and how do they support emotional health alongside physical health?
The PEP programs I lead - PC‑PEP, CancerPEP, PictouPEP, and the upcoming BreastCancerPEP—are digital, home‑based, and structured around a daily routine. They have been co-created with patients, communities, clinicians, and researchers, reflecting the belief that survivorship solutions must be built with the people they aim to serve. Participants receive short educational videos, guided meditations, strength and mobility training, sleep hygiene strategies, nutrition suggestions, emotional regulation skills, and relationship tools. That daily cadence creates stability and self‑efficacy; people often tell me they feel calmer, more grounded, and more hopeful within days. Emotional well‑being is woven into everything we do: breathing and mindfulness practices, gratitude and reframing exercises, storytelling and reflection, and relational and communication activities. I believe joy, play, relationships, and meaning are therapeutic.
Q: What drew you to patient empowerment—and was there a defining moment that shaped your approach?
My career has always centered on human resilience, but a pivotal moment came when a patient told me, “I feel lost on the inside and I don’t know where to begin.” He was receiving excellent clinical care and still felt alone and disoriented. That conversation crystallized my conviction that empowerment, building confidence, skills, and purpose, is not optional; it’s vital to healing. Since then, patients have been my greatest teachers. Their questions, fears, and triumphs guide everything I design and study. I am also profoundly grateful for the vision of Frank and Debbi Sobey, whose support made the Soillse Research Lab possible and helped change the landscape of survivorship research in Atlantic Canada and beyond. My collaborator and co‑lead, Dr. Rob Rutledge, has influenced my thinking through decades of compassionate practice. And my students, residents, postdocs, and trainees inspire me daily with their curiosity and commitment to patient‑centered care.
Q: What changes do you see in participants, and what does an ideal future of cancer care look like?
We consistently observe reductions in anxiety, depression, distress, and fear of recurrence, alongside improvements in sleep, strength, resilience, and self‑compassion. People reconnect with partners, return to hobbies, communicate more openly, and rediscover meaning and joy. One phrase we hear often is, “I feel like myself again.” My vision for the future is simple and ambitious: whole‑person supportive care as standard practice everywhere; digital platforms that augment - not replace - human connection; and empowerment recognized as a determinant of better clinical outcomes. Technology can enable personalized survivorship plans, continuous monitoring, digital coaching, remote access, and culturally tailored modules, but it must serve relationships, not supplant them.
Q: What’s next for your research—and what keeps you motivated?
We’re preparing the BreastCancerPEP Phase III randomized controlled trial, launching in 2026 (bcpep.org), to support women with non‑metastatic breast cancer. We’re expanding to new international sites (Australia, the UK, Denmark), continuing the Pan‑Canadian Movember PEP Trial focused on underserved communities, and working with government innovation agencies on next‑generation digital tools. At the same time, we’re publishing Phase 2, 3 and Phase 4 findings across PC‑PEP, CancerPEP, and PictouPEP, advancing PEP toward standard of care.
My motivation comes directly from patients. Every time someone says, “This program gave me hope again,” or “I feel like myself,” I am reminded why this work matters. As captured beautifully in our documentary Empower, if we are not helping people live fully, we may be missing the point.
Q: What might surprise people about your journey—and how do recognitions fit into the bigger picture?
People are often surprised by how much I value both care and competence — and how much joy I take in the creative work of helping patients feel whole again. What began with small patient groups and heartfelt conversations has grown into a global community that continues to guide us. Listening closely, asking the right questions, and learning directly from the people whose lives depend on this work shape everything I do. The true measure of impact is not an award or publication, but the moment a patient says, ‘I feel hope again.' That is when we know the work has truly reached the human heart.
