Stories
» Go to news mainE‑111 Intracranial carotid rupture during thrombectomy with effective tandem occlusion
New publication from Dr. Adela Cora, Dr. Matthias Schmidt and Dr. Robert Vandorpe. See full text.
Abstract
Introduction Mechanical thrombectomy has become the standard of care for patients presenting with acute ischemic stroke due to a large vessel occlusion. Intracranial hemorrhage is a serious complication which may occur during this procedure. The more commonly recognized cause of intraprocedural intracranial hemorrhage is due to iatrogenic vessel perforation. Here we present a series of patients with terminal ICA occlusions and proximal carotid stenosis that had mechanical thrombectomy complicated by devastating subarachnoid hemorrhage. Similarities between cases are highlighted and we hypothesize on the possible mechanism.
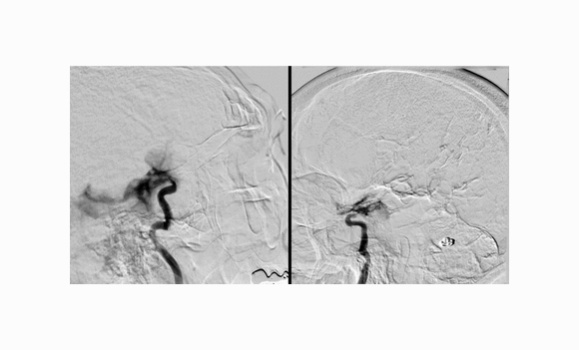
Case Description Three patients presented acutely with stroke symptoms due to an intracranial large vessel occlusion and had thrombectomy performed. Two of these patients had a tandem proximal and distal ICA occlusion extending to the M1 MCA with stenosis at the origin of the ICA. During the mechanical thrombectomy procedure all three patients had significant subarachnoid hemorrhage originating from the distal intracranial ICA in the region of the distal dural ring. The patient who did not have stenosis at the origin of the ICA, had the procedure performed with a balloon guiding catheter high in the cervical ICA which was relatively occlusive. Two patients had coiling performed to stop the hemorrhage, while the third patient was deemed for palliation. All three patients passed away within days after this serious complication.
Results We hypothesize that the cause of the subarachnoid hemorrhages in these patients was due to performing angiography in a closed system with the proximal stenosis/balloon guiding catheter causing blockage of the proximal ICA and the ICA terminus thrombus blocking the distal aspect. When performing an angiographic run, we hypothesize that the increased pressure can lead to rupture of the arterial wall at the weakest spot, which may be just past the distal dural ring where the ICA travels intracranially within the subarachnoid space.
Conclusion We highlight a newly encountered mechanism for potential injury to the distal ICA during mechanical thrombectomy. Sudden increase in pressure affecting the ICA in a system that is closed when performing angiography can rupture the distal ICA as it goes intracranially resulting in subarachnoid hemorrhage. It is important to be aware of this fatal complication when performing mechanical thrombectomy in patients with ICA terminus occlusion especially with proximal tandem carotid stenosis. Awareness of this complication will help operators to avoid performing angiographic runs in this potential closed space if not deemed necessary to avoid this potentially devastating complication.
Recent News
- Dr. Abraham receives CAIR Award
- Thank you to everyone who joined us for the 30th anniversary Radiology Research Day on May 8th!
- Nova Scotia’s Lung Screening Program expanding to Cape Breton, eastern mainland
- Donor‑supported nuclear medicine technology attracts top medical talent to the QEII
- Building Critical Skills at the Dalhousie Physician Leadership Workshop for Women in Radiology
- CAR/CSTR Practice Guideline on CT Screening for Lung Cancer
- CAR/CSACI Practice Guidance for Contrast Media Hypersensitivity
- CAR Practice Guideline on Bone Mineral Densitometry Reporting: 2024 Update
